
Ronald Jackups, MD, PhD, about the blood
supply at St. Louis Children’s Hospital.
Dr. Philip Spinella served twelve years in the United States military, including a year treating traumatic injuries in the 31st Combat Support Hospital in Baghdad. During his deployment, he was also part of a small group of physicians evaluating transfusion practices in treating hemorrhagic shock resulting from battlefield injuries.
Spinella co-authored multiple studies with others from his group indicating that transfusion of red blood cells stored for a prolonged period may be associated with an increase in complications and mortality. One such report concluded that fresh whole blood was preferable to the stored blood components (red cells, platelets, and plasma) that had been shipped from the states. These cells had been stored for longer than 21 days, with median storage time of 33 days. The report concluded that while the risk of viral infection from fresh blood was very slightly higher even after prescreening, fresh whole blood was superior to aged cells in terms of improved physiological effects such as cardiac output and better clinical outcomes.
Now associate professor of pediatrics at Washington University Medical School, and director of the pediatric Blood Research Program, he continues to question how well red blood cells maintain their safety and functionality after relatively long storage. He is specifically interested in the question as it relates to growing children who are critically ill.
Are fresh red blood cells superior in treating critically ill children?
Spinella has received a $7.8 million NIH grant to study whether the age of transfused red blood cells in critically ill children affects the risk of new or progressive multiple organ failure. His co-investigator is Dr. Marisa Tucci of Sainte-Justine Hospital in Montreal.
Normally, children in the United States requiring transfusions are given the oldest available blood, the standard blood banking practice. Storage time averages 17-21 days, and ranges from 2 to 42 days for children. In St. Louis Children’s hospital and many other medical centers, certain patients are always given fresh blood products—babies less than six months old, children having cardiac surgery, and certain children with sickle cell anemia.
In this five-year study, 1538 critically ill children from 3 days to 16 years of age will be divided into two groups. One group will receive on a random basis fresh red blood cells, defined as having been stored less than one week. The other half of the will be treated with the standard transfusion protocol as described. Among the pediatric intensive care unit patients would be those post-operative, septic, and victims of trauma. Those who would already receive fresh red blood cell transfusions will not be included in the study, nor will patients whose parents have not given permission for participation.
About thirty medical centers in the U.S. and Canada will participate in the study. The Canadian Institutes of Health research is funding Canada-based costs.
Only blood bank personnel will know which patients have received fresh vs. standard red blood cells. The label indicating length of storage will be obscured in the blood bank; such an experiment in which neither patient nor doctor knows the which kind of blood is given is called “double-blind.”
Lack of clinical proof on clinical efficacy of older red blood cells
Red Blood Cells
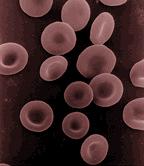 Red cells are the most abundant cells in the blood—5-6 million per cubic millimeter, or about 25 trillion in the total circulation. Their single function is to carry oxygen from the lungs to the tissues and then carry carbon dioxide back to the lungs to be exhaled.
Red cells are the most abundant cells in the blood—5-6 million per cubic millimeter, or about 25 trillion in the total circulation. Their single function is to carry oxygen from the lungs to the tissues and then carry carbon dioxide back to the lungs to be exhaled.
Essentially containers for hemoglobin, red cells have unique characteristics to optimize their function.
- Red blood cells are nearly uniform in size and shape. A concavity on both sides of the disc allows for maximal gas exchange.
- Mature red cells have no nucleus and cannot divide
- Red cells have no mitochondria, the intracellular structures that use oxygen in producing biochemical energy. Instead, red cells metabolize anaerobically, and produce little biochemical energy.
For Spinella, the questions centers on a policy decision. When the Food and Drug Administration changed its standards for new drug approval to tests of both safety and efficacy, blood products were “grandfathered”. That is, blood products had to pass strict safety standards of survival in the circulation, but were not required to pass tests demonstrating function. New formulations for red cell storage solutions doubled the time that cells could be stored and transfused safely according to those decades-old standards. However, blood processors were not required to show that these older cells could take up and release oxygen as well as fresh cells when transfused.
“It’s like thinking you have a good car because the body is intact. But if the engine does not work, the car is not very functional. The red cells circulate intact, but we have no idea if, when they’re stored for 42 day or close to that, they actually deliver oxygen the way we think they should.”
Laboratory studies have repeatedly shown that red blood cells do change in storage. For instance, by 14 days, they lose flexibility. Oxygen exchange occurs in capillaries, rather than in veins and arteries. As the cells move through the narrow capillaries, they undergo changes of shape. Can rigid cells get into and move through capillaries? The cells do regain flexibility after a day or so; obviously at least in this respect, the cells can serve in non-emergency situations.
Other changes with storage, having to do with energy metabolism, clotting, and immune function, have been well documented in the laboratory also.
Results will be important to blood banks
Increased storage times are important in blood banking in terms of maintaining inventory. As a general practice, the Red Cross sends red cells on request to hospital blood banks. If the cells are not used by 35 days, as may happen in rural areas, they are redistributed to large urban medical centers, including St. Louis Children’s Hospital. In these large centers, demand is great, and the blood is less likely to be wasted.
A Short History of Blood Banking
The possibility of blood banking began about one hundred years ago with the discovery that salts of citric acid could keep human blood from coagulating. Addition of glucose to the solution provided energy. In 1917, Dr. Oswald Robertson transfused human blood that had been refrigerated and stored in citrate-glucose for 26 days to soldiers in Flanders during World War 1.
The introduction of plastic bags for blood collection in 1950 not only reduced the weight and breakage of transported blood, but also had the unexpected side effect of reducing hemolysis (breakage of red cells) because of a chemical leached from the plastic.
The plastic bag allowed safer storage of red cells separated from plasma. Today most transfusions use the cells packed down after centrifugation. Normally, the leukocytes (white blood cells)are removed, because they are nucleated cells that can secrete various biochemical agents, including enzymes that digest proteins. Removing leukocytes also prevents immunological complications.
Modern red blood cell preparations contain several additives that serve to prolong shelf life.
There is not universal agreement in the transfusion literature that length of blood storage correlates with adverse results clinically. This study is significant because it is the first large double-blind investigation on children in pediatric intensive care units.
Dr. Ronald Jackups, who will be in charge of the blood banking at Children’s Hospital during the study, summarizes the significance this way: “This is the first study of its kind in this particular population, who typically require a lot of transfusions, and are at higher risk of transfusion-related complications. If long storage times do have a negative effect on patient outcomes, it could seriously affect our ability to preserve our supply of blood.
Think of it like a grocery store stocking milk. If all the expiration dates on milk were cut in half, because it was shown that milk stored that long was unsafe, stores would have to stock less milk at any point in time in order to avoid wasting it, which subsequently could lead to shortages. Thus, we should only shorten expiration dates on blood if there’s proof that older products are truly more dangerous. We need large studies like these one to answer that question once and for all.”
Spinella would point out that large studies would also be appropriate to show efficacy if new formulas for red cell storage should be adopted.
The American Red Cross supplies blood to Children’s Hospital bank. Dan Fox, local communications program manager, states “The Red Cross welcomes this study and should evidence indicate a need for change in current practices, the Red Cross will use the best available science to provide the safest possible blood for patients.”
This article was originally published in the St. Louis Beacon.
